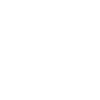
Hawai‘i Ranks High in Healthcare Improvement Report
Hawai‘i ranked in the top quartile with 11 other states that showed improved healthcare and expanded access in 2015.
Stark differences in performance persisted among states on many indicators. In the overall rankings, the leading and lagging states remained the same. Minnesota, Vermont, Hawai‘i and Massachusetts again ranked at the top. The four lowest-ranking states were Louisiana, Arkansas, Oklahoma and Mississippi.
According to the Commonwealth Fund’s 2015 state healthcare system scorecard, healthcare systems in the US improved more than they declined since 2014 and access to healthcare expanded across the nation.
The latest edition of the state scorecard—the first one in the Commonwealth Fund’s series to reflect a full year of the Affordable Care Act’s major health insurance expansions—finds that the uninsured rate for working-age adults declined in nearly every state between 2013 and 2014 (Massachusetts, which already had the nation’s lowest uninsured rate, saw no change). In 39 states, the rate dropped three percentage points or more.
Results from a Scorecard on State Health System Performance, 2015 Edition, ranks the healthcare systems of every state and the District of Columbia based on 42 indicators of healthcare access, quality, costs and outcomes. Thirty-six of the 42 indicators are used to reveal trends over time. In addition to the scorecard, there is an online interactive map enabling users to view and compare states’ scorecard results.
Four low performing states improved on a number of measures: Louisiana on 16, Oklahoma on 14, and Kentucky and Tennessee on 13. Tennessee didn’t lose ground on any measure. Colorado, Florida, Kansas, New York, North Carolina, Missouri and South Carolina each got worse on only one measure, while improving on between six and 10 measures.
“These are the most substantial and widespread state improvements in access to care we’ve seen since we created the state scorecard series in 2007,” said Commonwealth Fund President David Blumenthal, MD. “While there are still wide differences among states, and performance has worsened in some instances, policy changes like those in the Affordable Care Act, incentives to improve healthcare quality and safety, and provider-led efforts are beginning to bear fruit.”
Access to Care Improves Substantially
The state-by-state impact of expanded access to care is detailed in a separate Commonwealth Fund brief, The Changing Landscape of Health Care Coverage and Access: Comparing States’ Progress in the ACA’s First Year.
In addition to substantial gains in health insurance coverage for adults, the uninsured rate for children age 18 and under fell in a majority of states and declined by at least two percentage points in 16 states. In addition, adults in 2014 were less likely than in the previous year to say that costs stopped them from going to a doctor when they needed healthcare, with 21 states seeing an improvement of two percentage points or more on this indicator.
There was an almost six-fold difference in uninsured rates for low-income working-age adults across the states, ranging from 8% in Massachusetts to 46% in Texas. Nevertheless, substantial shares of low-income adults gained health insurance:
In 2014, the share of low-income adults who were uninsured dropped three percentage points or more in every state except Maine, where it fell two percentage points.
The uninsured rate for low-income adults decreased the most (13 to 18 percentage points) in states that had expanded their Medicaid programs by January 2014: Kentucky, Washington, West Virginia, Oregon, Rhode Island and Nevada.
Additional Scorecard Findings on Quality and Preventive Care
In 23 states, hospital readmission rates fell by two percentage points or more among Medicare beneficiaries who were discharged from the hospital and sent to skilled nursing facilities for post-acute care. Looking nationwide at all Medicare enrollees, the scorecard found a reduction in hospital readmissions that accelerated when the Medicare program began financially penalizing hospitals with high rates of readmissions in 2012. The states that had the highest readmission rates saw some of the biggest declines.
In 45 states, patients hospitalized for heart attack, heart failure or pneumonia were substantially less likely to die within 30 days of their hospital stay compared to an earlier measurement baseline.
In 35 states, there was a reduction of at least three percentage points between 2011 and 2012 in the share of elderly Medicare beneficiaries receiving a high-risk prescription medication that experts say older people should avoid.
Across the states, there were gains and losses in childhood vaccination rates: the percentage of children between 19 months and 35 months who were up to date on all of their vaccines increased by three percentage points or more in 22 states but dropped by a similar amount in 15 states and the District of Columbia.
Less than half of adults age 50 and older are receiving all of the cancer screenings and vaccinations that experts recommend. The preventive care rate dropped 2 percentage points or more in 15 states.
“The scorecard shows us that when it comes to your healthcare, where you live matters—but that doesn’t have to be the case,” said Douglas McCarthy, senior research director at the Commonwealth Fund and lead author of the report. “Research has shown that even where resources are limited, strong leadership and collaboration among providers, policymakers, health plans, public health agencies, businesses and others can lead to improvement that ensures all of us have the opportunity to benefit from a strong and thriving healthcare system.”
Moving Forward
According to the scorecard, improvements at the state level would have substantial national impact. If every state were to do as well as the best-performing state, 84,000 early deaths would be prevented, 8 million additional older adults would get recommended preventive care, and 24 million more people would have health insurance.
The authors note that the progress many states have made, particularly in access to care, is evidence that strong polices and federal and state leadership can pave the way for improvements. Programs initiated by the Affordable Care Act, for example, offer states opportunities to partner with the federal government on implementing a variety of innovations, such as Medicaid “health homes” for people with chronic conditions and care integration programs for dually eligible Medicaid–Medicare beneficiaries, a population with particularly complex health needs. State and local policies can also support healthy living in the community, enabling everyone a better chance for a long and healthy life.
The complete scorecard report is available online.